Periodontitis is a serious gum disease that silently attacks your oral health. Unlike a regular cavity or toothache, periodontitis doesn’t always hurt, until it’s too late. If left untreated, it can lead to gum recession, bone loss, and even tooth loss.
Table of Contents
ToggleIn Canada, nearly 7 out of 10 adults suffer from some form of gum disease, and periodontitis is the advanced stage. This prevalence underscores the importance of early detection and the right treatment, empowering you to take control of your oral health.
Let’s explore the four major symptoms of periodontitis, how it develops, and how you can take charge of your gum health with the help of general dentistry in Woodbridge.
4 Major Symptoms of Periodontitis

1. Bleeding or Swollen Gums
If your gums bleed when you brush or floss, it’s not “normal” it’s an early sign of periodontitis. Swelling, redness, or tenderness also indicate inflammation, which means your body is fighting infection.
Over time, untreated inflammation allows bacteria to penetrate deeper into your gums, forming pockets that collect more plaque and worsen the condition.
Action Tip: If your gums bleed more than once a week, it’s crucial to schedule a check-up with your dentist right away, ideally within the next few days, to prevent the condition from worsening.
2. Persistent Bad Breath
Constant bad breath isn’t just embarrassing, it’s often caused by bacteria hiding deep in the gum pockets, a hallmark of gum disease. This bacteria releases toxins that not only cause odor but also damage gum tissue.
Mouthwash can only mask the problem. The root cause requires professional cleaning and periodontitis treatment.
3. Gum Recession or “Longer” Teeth
When gums begin to recede, it’s often due to the destruction of the supporting tissue and bone caused by periodontitis. You may notice your teeth appearing longer or feel more sensitivity to hot or cold.
This stage of gum recession can be slowed or stopped, but reversing it often requires advanced procedures like oral surgery in Woodbridge. These procedures, performed by experienced professionals, aim to restore lost tissue and bone, and are often the last resort when other treatments have not been successful.
4. Loose or Shifting Teeth
As periodontitis progresses, it eats away at the bone structure holding your teeth in place. This leads to loosening teeth, bite misalignment, or even tooth loss.
When teeth begin to shift or feel wobbly, the disease has reached a critical point. Seeking help from general dentistry in Woodbridge is essential before the damage becomes irreversible.
4 Periodontal Disease Stages
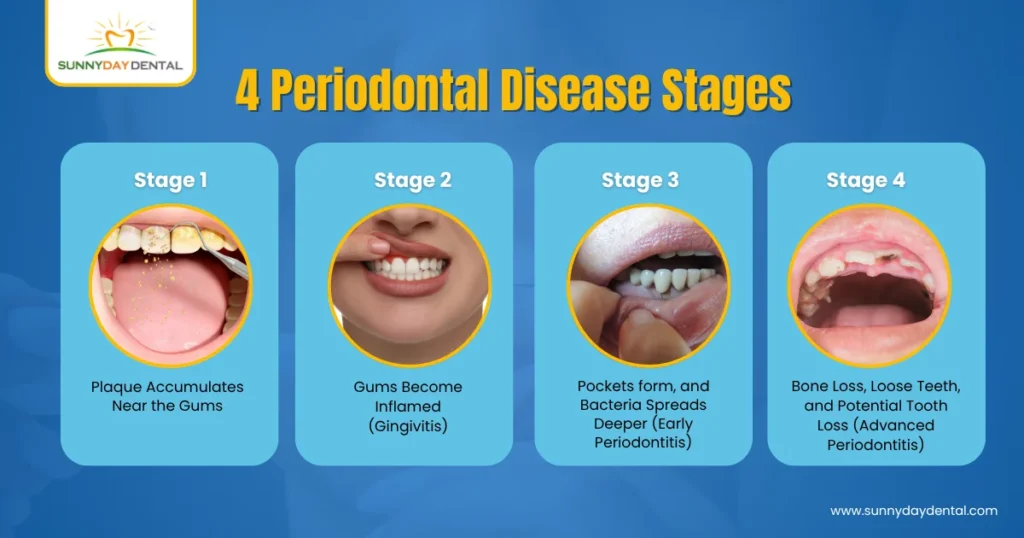
Plaque buildup is the primary cause of periodontitis. When plaque hardens into tartar, it can only be removed by professional dental cleaning. If left untreated, this tartar leads to gum inflammation (gingivitis) and eventually periodontitis.
Here’s how the disease typically progresses:
- Stage 1: Plaque accumulates near the gums
- Stage 2: Gums become inflamed (gingivitis)
- Stage 3: Pockets form, and bacteria spreads deeper (early periodontitis)
- Stage 4: Bone loss, loose teeth, and potential tooth loss (advanced periodontitis)
9 Common Risk Factors for Gum Disease

Several factors can increase your risk of developing gum (periodontal) disease. While poor oral hygiene is the leading cause, other health conditions and lifestyle habits can also play a role. Understanding these risk factors can help you take steps to prevent or manage the condition.
Common Risk Factors for Gum Disease:
- Poor oral Hygiene Habits: Infrequent brushing or flossing allows plaque and tartar to build up along the gumline.
- Smoking or Tobacco Use: One of the most significant risk factors. Smoking weakens your immune system and reduces blood flow to the gums, making it harder for your body to fight infection.
- Hormonal Changes: Pregnancy, menopause, or puberty can make gums more sensitive and prone to inflammation.
- Chronic Health Conditions: Diabetes, heart disease, and conditions that affect the immune system may increase susceptibility to gum infections.
- Genetics: Some people may be more prone to gum disease due to inherited traits.
- Certain Medications: Drugs that reduce saliva flow, cause dry mouth, or affect gum tissue (like some anti-seizure or blood pressure medications) can contribute to gum problems.
- Stress: High stress levels can weaken your immune system and interfere with your ability to fight infection.
- Poor nutrition: A diet lacking in essential nutrients, especially vitamin C, can impair gum health.
- Clenching or grinding teeth: This can put excess pressure on the tissues supporting your teeth, potentially speeding up gum deterioration.
If you have one or more of these risk factors, it’s important to maintain a regular dental checkup schedule and follow good oral hygiene practices. Your dentist is here to help you. Early intervention can prevent minor gum issues from progressing into serious disease, giving you peace of mind about your oral health.
4 Treatment Options: How to Save Your Gums from Periodontitis
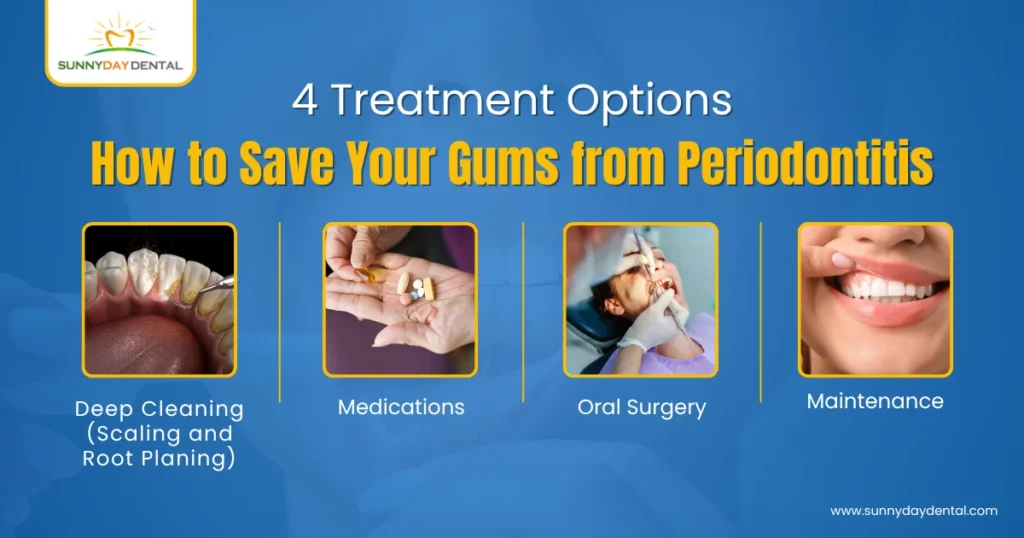
1. Deep Cleaning (Scaling and Root Planing)
This non-surgical treatment involves cleaning below the gumline to remove plaque and tartar from pockets around teeth. It allows gums to heal and reattach to the tooth surface.
2. Medications
Antibiotics may be placed directly into the gum pockets or prescribed to control infection.
3. Oral Surgery
In advanced stages, oral surgery in Woodbridge, such as flap surgery or bone grafting, may be necessary to restore lost tissue and bone.
4. Maintenance
Once treated, periodontitis needs lifelong maintenance. Regular visits to your dentist and a disciplined oral hygiene routine are key.
How to Prevent Periodontitis
- Brush twice daily using fluoride toothpaste
- Floss once a day to clean between teeth
- Get regular professional cleanings every 6 months
- Avoid smoking, which increases your risk
- Watch for signs like bleeding gums or loose teeth
With the help of a general dentist in Woodbridge, you can catch early signs of gum disease and prevent serious complications.
Summing Up – What are the Symptoms of Periodontitis?
The four common symptoms of periodontitis are swollen or bleeding gums, persistent bad breath, gum recession, and loose teeth. Early diagnosis and professional periodontitis treatment can prevent permanent damage.
Don’t Wait for the Pain to Start
Unlike a toothache, periodontitis often progresses without pain. That’s why prevention and early diagnosis are crucial. By the time you feel discomfort, your gums may already be severely damaged.
At Sunny Day Dental, we use advanced imaging and diagnostic tools to detect gum disease in its earliest stages. Whether you need basic cleaning or periodontitis treatment, our expert team ensures your smile stays healthy and confident.
Save Your Gums with Expert Care at Sunny Day Dental
Early signs of periodontitis, like bleeding gums or bad breath, should never be ignored.
Sunny Day Dental in Woodbridge offers trusted, advanced gum care to protect your smile.
- Specialized treatment for periodontitis and gum disease
- Deep cleaning (scaling & root planing) to stop disease progression
- Oral surgery options available for advanced cases
- Friendly, local experts in General Dentistry in Woodbridge
FAQs About Periodontitis (Gum Disease)
1. Can periodontitis be cured completely?
Periodontitis cannot be “cured” in the traditional sense once it’s advanced, but it can be effectively managed. With proper periodontitis treatment, professional cleanings, and good oral hygiene, the disease can be controlled, and further damage can be prevented.
2. How often should I visit the dentist if I’ve had periodontitis?
After treatment, patients are generally recommended to visit their dentist every 3 to 4 months for maintenance therapy. These frequent check-ups help remove buildup and monitor the condition to prevent relapse.
3. Is periodontitis contagious?
While periodontitis itself isn’t contagious, the bacteria that cause it can be passed through saliva. This means activities like sharing utensils or kissing can transfer harmful bacteria, especially in families or couples.
4. What’s the link between periodontitis and other health problems?
Studies show that periodontitis may increase the risk of heart disease, diabetes, and even complications during pregnancy. This is because inflammation from gum disease can impact your body’s overall immune response and circulatory health.
5. Do I need surgery if I have periodontitis?
Not always. Many cases of periodontitis can be managed through non-surgical methods like scaling and root planing. However, if the disease is advanced and bone loss is significant, oral surgery in Woodbridge may be recommended to restore support to your teeth.