For most people, wisdom teeth are just late arrivals that cause some discomfort and then get removed. But in some cases, impacted wisdom teeth, those that fail to emerge properly, can lead to more serious oral health problems.
Table of Contents
TogglePatients often ask whether this trapped tooth tissue can cause or contribute to oral cancer risk factors. The short answer: not directly, but indirectly it can create conditions that raise risk.
Let’s break down what that means and why regular dental checks are crucial for prevention.
What Are Impacted Wisdom Teeth

Wisdom teeth are the third set of molars, usually erupting between ages 17 and 25. When there’s not enough space in the jaw, they become impacted, meaning they stay trapped under gum tissue or bone.
There are two main types:
- Soft tissue impaction: The tooth is partially visible but covered by gum.
- Bony impaction: The tooth is entirely trapped beneath bone.
Both forms can lead to wisdom tooth complications, such as infection, decay, and gum inflammation — and these chronic issues can increase inflammation in surrounding tissue, creating a risky environment over time.
4 Ways How Chronic Inflammation Links to Oral Cancer Risk
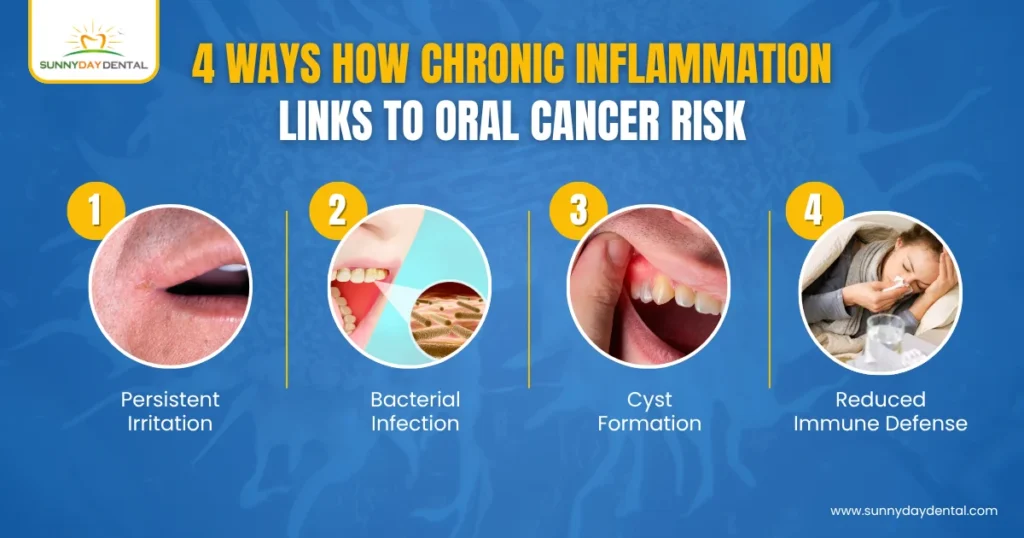
While impacted wisdom teeth themselves are not cancerous, ongoing infection or irritation in that area can heighten oral cancer risk factors.
Here’s how:
- Persistent Irritation: An impacted tooth that rubs against the cheek or gum can cause chronic trauma. Over years, this can lead to tissue changes.
- Bacterial Infection: When food and bacteria collect under gum flaps, they produce toxins that damage nearby cells.
- Cyst Formation: Fluid-filled sacs (dentigerous cysts) can form around impacted teeth. Though benign, some can become aggressive or transform into rare jaw tumors if untreated.
- Reduced Immune Defense: Ongoing inflammation keeps local immunity low, allowing precancerous changes to develop more easily.
Research from the Canadian Cancer Society identifies chronic irritation and infections as potential oral cancer risk factors, especially when combined with smoking, alcohol use, or HPV exposure.
Impacted Wisdom Tooth – 5 Early Warning Signs to Watch For
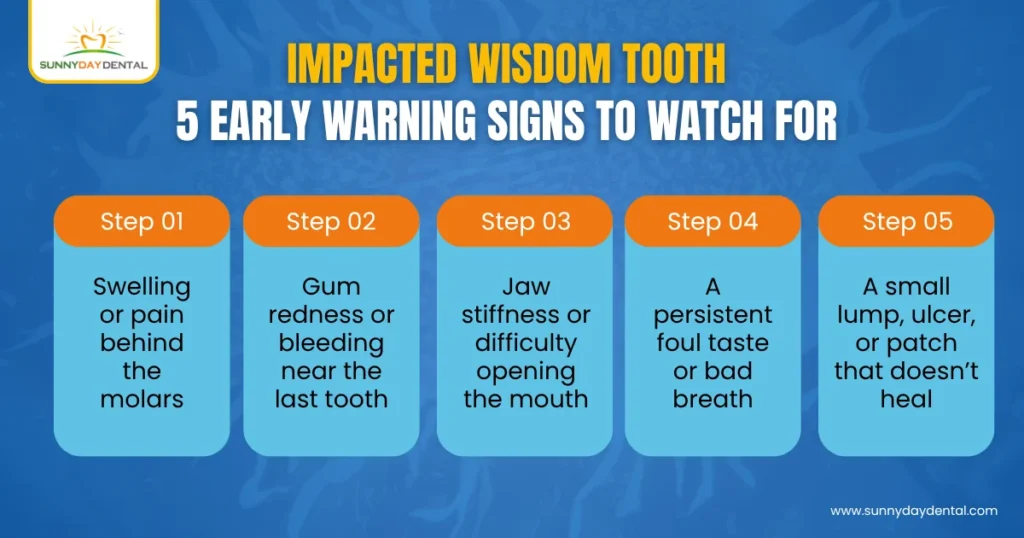
Because impacted teeth often stay hidden, symptoms can go unnoticed until complications develop. See your emergency dentist in Woodbridge if you experience:
- Swelling or pain behind the molars
- Gum redness or bleeding near the last tooth
- Jaw stiffness or difficulty opening the mouth
- A persistent foul taste or bad breath
- A small lump, ulcer, or patch that doesn’t heal
Persistent lesions near the jawline or cheek area should always be examined — early evaluation can rule out serious issues long before they progress.
Common Complications from Untreated Impaction
Beyond cancer-related concerns, wisdom tooth complications can include:
- Pericoronitis: Infection of the gum flap covering a partially erupted tooth
- Bone loss or cysts: Damage to surrounding bone tissue
- Tooth decay: Difficulty cleaning leads to cavities in the molars next to the wisdom tooth
- Nerve compression: Some impacted teeth sit close to the inferior alveolar nerve, causing numbness or tingling in the jaw
These issues are treatable, but delay increases both pain and risk. That’s why proactive dental imaging and removal are so strongly advised.
4 Conditions that Aggravate the Risk of Oral Cancer from Impacted Wisdom Teeth
Certain habits and health conditions can amplify how impacted wisdom teeth affect oral health:
- Tobacco and Alcohol Use: Both are major oral cancer risk factors. When paired with chronic infection, the risk multiplies.
- Family History: If oral or head-neck cancers run in your family, inflammation control becomes even more critical.
- Poor oral Hygiene: Bacteria around impacted teeth can thrive unnoticed.
- HPV Infection: Some strains of HPV (especially 16 and 18) increase oral cancer risk; chronic gum injury can worsen exposure effects.
Even without these risk factors, untreated impactions often lead to costly restorative work later.
Prevention: The Role of Early Diagnosis
Regular dental X-rays can spot developing impactions before they cause pain or damage. At Sunny Day Dental, panoramic imaging is part of every young adult’s preventive plan — so potential impactions can be managed before they turn problematic.
Early removal is simpler, heals faster, and prevents the long-term inflammation linked to oral cancer risk factors.
If your wisdom teeth are already causing discomfort, your dentist may recommend extraction under local or sedation anesthesia, followed by antibiotic and pain management care.
How Dentists Evaluate for Oral Cancer

Checking for oral cancer isn’t a one-time task; it’s part of every comprehensive dental exam. Here’s what’s typically done:
- Visual Screening: Looking for white or red patches, ulcers, or thickened tissue.
- Palpation: Gently feeling for lumps along the neck and jawline.
- Imaging: Scans to check for cysts or bone lesions near impacted wisdom teeth.
- Biopsy Referral: If a suspicious area is found, a small tissue sample may be taken for lab testing.
Regular screening ensures that even subtle changes are detected early.
Can Impacted Wisdom Teeth Directly Cause Oral Cancer
No. Impacted wisdom teeth do not directly cause cancer. However, chronic inflammation and tissue irritation caused by infection or trauma in that area can be a contributing factor in some cases.
It’s similar to how long-term gum disease or ill-fitting dentures can create an environment that encourages abnormal cell changes over time. The best prevention is consistency: hygiene, checkups, and early removal when needed.
A Simple Step for Long-Term Protection
It’s easy to ignore wisdom teeth when they are not painful, but leaving impacted wisdom teeth untreated can silently harm your gums and jaw, and increase your exposure to avoidable risk factors over time.
Early monitoring and removal, paired with regular oral cancer screenings, are two of the most powerful preventive steps you can take.
Prevent the Oral Cancer from Impacted Wisdom Teeth with Sunny Day Dental

If you suspect your wisdom teeth are impacted or notice recurring discomfort near the back of your mouth, schedule an evaluation.
At Sunny Day Dental in Woodbridge, we provide precise diagnosis, gentle extractions, and long-term preventive care to reduce infection and lower oral cancer risk factors for every patient.
Book your assessment or call our emergency dentist in Woodbridge to get checked before minor irritation turns into a chronic problem.
FAQs About Impacted Wisdom Teeth and Oral Cancer
1. Can impacted teeth turn cancerous themselves?
No, teeth do not become cancerous. But the surrounding tissue can undergo precancerous changes if exposed to chronic irritation or infection.
2. What are the most common oral cancer risk factors?
Tobacco use, alcohol, HPV infection, poor diet, and chronic inflammation are the top contributors.
3. How do I know if I have impacted wisdom teeth?
X-rays during your dental checkups will reveal impaction before pain starts.
4. When should I see an emergency dentist in Woodbridge?
If you have swelling, pain, or a sore behind the molars that does not heal in two weeks, see a dentist right away.
5. Can removing impacted wisdom teeth reduce oral cancer risk?
Indirectly, yes. By removing a constant source of irritation and infection, you reduce the overall inflammation load on surrounding tissue.


