Living with diabetes often means questioning whether certain medical or dental procedures are safe. One of the most common concerns I hear in my practice is whether dental implants for diabetes are a realistic and safe option. Tooth loss affects confidence, nutrition, and overall health, and dental implants remain the gold standard for replacing missing teeth.
Table of Contents
ToggleThe good news is that modern dentistry has made dental implants more accessible than ever, even for people managing diabetes.
This blog will walk you through everything you need to know, from safety and success rates to preparation, healing, and long-term care. Whether you are newly diagnosed or have been managing diabetes for years, this article is designed to help you make informed, confident decisions.
What is the Link Between Diabetes and Oral Health?

Diabetes not only affects blood sugar levels, it also has a direct impact on oral health. Poorly controlled diabetes can reduce the body’s ability to fight infection and slow healing. This is why people often wonder if dental implants for diabetes are risky.
High blood glucose can increase the risk of gum disease, bone loss, dry mouth, and delayed wound healing. However, when diabetes is well managed, the mouth can heal just as effectively as in non diabetic patients. Today, dental professionals evaluate overall health rather than excluding patients based on diagnosis alone.
Can People with Diabetes Safely Get Dental Implants?
Yes, people with diabetes can safely receive dental implants when their condition is well-controlled. The key lies in proper planning, medical coordination, and strict oral hygiene. Many patients ask, can diabetics get dental implants, and the answer is increasingly positive thanks to advances in implant technology and surgical techniques.
Recent clinical studies published between 2023 and 2025 show implant success rates above 90% in patients with controlled diabetes. This places dental implants for diabetes close to the success rates seen in non diabetic individuals.
The decision is not based on diabetes alone, but on how well blood sugar levels are managed over time.
The Role of HbA1c Levels in Implant Success
HbA1c is one of the most important markers dentists consider before recommending implants. It reflects your average blood sugar levels over the past two to three months. Patients often search for guidance on HbA1c implants, and for good reason.
Most dental professionals prefer HbA1c levels below 7% before implant surgery. Levels between 7 and 8 may still be acceptable with added precautions, while levels above 8 usually require medical optimization first.
Maintaining stable HbA1c levels improves bone integration, reduces infection risk, and increases the long term success of dental implants for diabetes.
Dental Implants and Type 2 Diabetes
Type 2 diabetes is the most common form seen in dental clinics. Patients often ask about dental implants, diabetes type 2 diabetes, and whether insulin resistance affects implant outcomes.
The encouraging news is that patients with well-managed type 2 diabetes experience excellent results. Modern implant surfaces promote faster bone integration, even in patients with metabolic challenges. What matters most is consistency in blood sugar control rather than the type of diabetes itself.
When managed responsibly, dental implants for diabetes in type 2 patients can last decades.
How Dental Implants Work in Diabetic Patients
Dental implants are titanium posts placed into the jawbone to replace missing tooth roots. Over time, the bone fuses to the implant in a process called osseointegration. For diabetic patients, this process may take slightly longer, but it remains predictable when blood sugar is controlled.
This is why thorough evaluation and personalized planning are essential. With the right approach, dental implants for diabetes provide stability, function, and confidence that dentures cannot match.
Step-by-Step Guide to Getting Dental Implants with Diabetes
Before starting treatment, it helps to understand what the journey looks like. Below is a practical, patient focused roadmap designed to remove uncertainty and build confidence.
1. Before Implant Surgery
Preparation sets the foundation for success. A proactive approach significantly improves outcomes for diabetic patients.
- Comprehensive medical history review and physician coordination
- HbA1c testing and blood sugar assessment
- Gum disease evaluation and treatment if needed
- Digital imaging to assess bone quality
- Personalized implant planning
These steps ensure your body is ready to support dental implants for diabetes and reduce preventable risks.
2. During Implant Placement
The surgical phase is precise and minimally invasive when performed by experienced clinicians. Modern techniques reduce trauma and support faster healing.
- Use of guided implant placement technology
- Local anesthesia with careful monitoring
- Antibiotic protocols when appropriate
- Gentle surgical techniques to protect bone
This stage is designed to support safe placement and long term stability for dental implants for diabetes.
3. After Surgery and Healing
Healing is where commitment truly matters. Diabetic patients who follow post operative instructions closely achieve the best results.
- Blood sugar monitoring during recovery
- Excellent oral hygiene practices
- Soft food diet during early healing
- Regular follow up appointments
With proper care, dental implants for diabetes integrate successfully and restore full oral function.
Risks and How to Reduce Them
Every surgical procedure carries some risk, but most concerns can be minimized with preparation and professional care. Understanding risks empowers patients rather than discourages them.
Potential risks include delayed healing, infection, and implant failure. These risks increase when diabetes is uncontrolled. However, proactive management dramatically reduces complications.
Dentists trained in treating medically complex patients know how to tailor dental implants for diabetes to individual needs.
4 Long Term Benefits of Dental Implants for Diabetic Patients
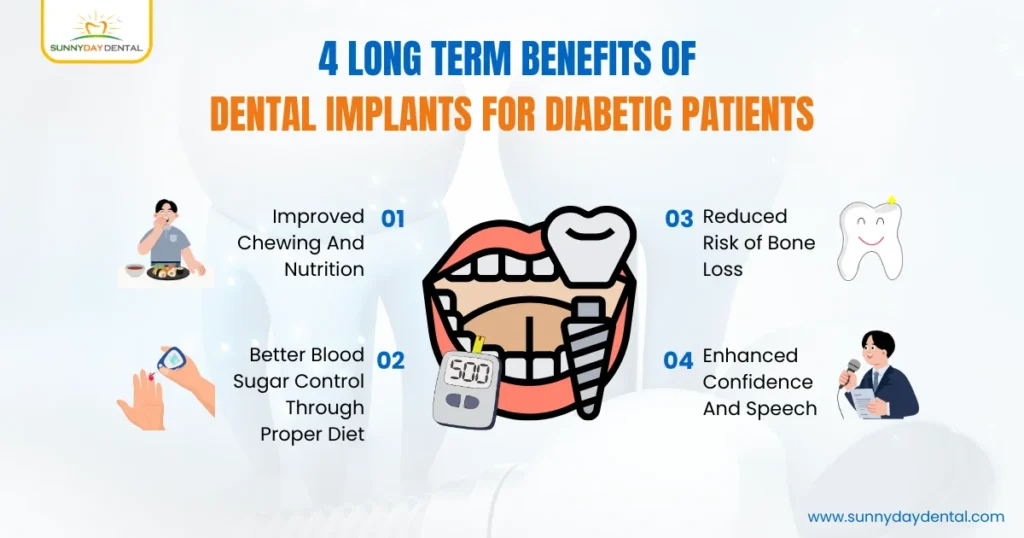
Dental implants offer more than aesthetic improvements. They directly support overall health and quality of life.
- Improved chewing and nutrition
- Better blood sugar control through proper diet
- Reduced risk of bone loss
- Enhanced confidence and speech
For many patients, dental implants for diabetes become a life changing investment in health and well-being.
Considering Dental Implants with Diabetes in Woodbridge? Sunny Day Dental Can Help

At Sunny Day Dental, we provide expert care for people seeking dental implants in Woodbridge, including those managing diabetes. We focus on the link between blood sugar control, oral health, and implant success so you can make confident, informed decisions.
Every treatment is planned using advanced diagnostics and evidence-based protocols, with careful review of your medical history to ensure safe healing and long-term results.
Book your personalized consultation today and take the first step toward a healthier, more confident smile.
FAQs About Dental Implants for People with Diabetes
1. Can dental implants affect blood sugar levels?
Dental implants themselves do not affect blood sugar. However, improved chewing can support better nutrition, which may help stabilize glucose levels over time.
2. Is implant surgery painful for diabetic patients?
Implant surgery is generally comfortable with local anaesthesia. Discomfort after surgery is manageable and similar to that of non-diabetic patients when healing is monitored properly.
3. How long do implants last in people with diabetes?
With good oral hygiene and controlled diabetes, implants can last 20 years or longer. Consistent dental visits are key.
4. Do diabetic patients need special implant materials?
Standard titanium implants work well for diabetic patients. Some surface-treated implants may promote faster bone integration.
5. Can implants help prevent further tooth loss?
Yes, implants stabilise the jawbone and prevent bone loss that can occur after missing teeth, supporting long-term oral health.